The U.S. Food and Drug Administration announced on Wednesday that food manufacturers who intentionally use sesame in their products and properly disclose it on labels are not in violation of a new federal food allergy law.
The Center for Science in the Public Interest, a food safety advocacy group, had raised concerns about the unintended outcome of the January law, which led to an increase in companies incorporating sesame into foods that previously did not contain it. However, the FDA rejected the advocacy group’s appeal to stop this practice.
According to food allergy experts, over 1.6 million people in the U.S. suffer from sesame allergies, and these allergies can result in severe and potentially fatal reactions.
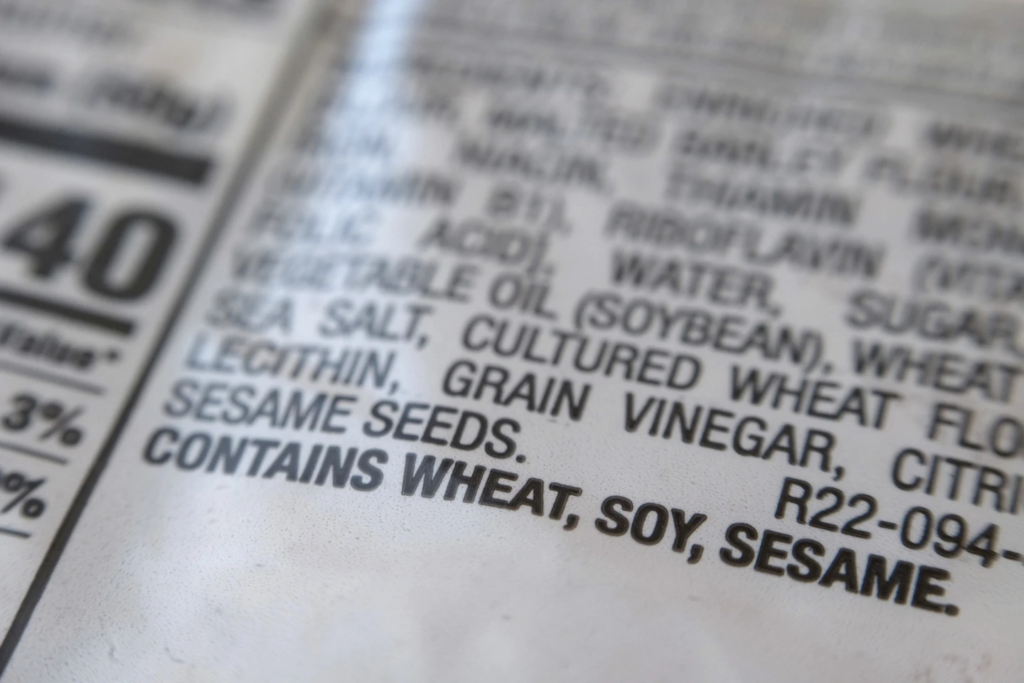
Indeed, sesame can be found in various forms and products, not just limited to the obvious ones like sesame seeds on hamburger buns. It serves as a significant ingredient in a wide range of foods, including protein bars, ice cream, and can even be added to sauces and spice mixes. Due to its versatile nature and potential health benefits, sesame finds its way into numerous culinary creations and packaged goods. However, it’s essential for individuals with sesame allergies to be vigilant about checking labels and avoiding products that may contain this allergen to prevent any adverse reactions.
Sesame has become increasingly prevalent in various food products, including those from popular restaurant chains such as Olive Garden, Chick-Fil-A, and Wendy’s, as well as bread makers supplying grocery stores and schools. The rationale behind this trend is that complying with the strict federal regulations to prevent cross-contamination has proven to be challenging. As a result, adding sesame to products and clearly labeling it has become an easier solution for producers than attempting to keep sesame out of other foods and away from shared equipment.
However, food safety advocates express concern over this practice, highlighting the potential dangers it poses to individuals with sesame allergies. They argue that the widespread use of sesame limits the choices available to people with allergies and increases the risk of accidental exposure, which can lead to severe allergic reactions.
Robert Earl, the vice president of regulatory affairs for the nonprofit group Food Allergy Research & Education, has received reports of allergic reactions occurring after people with sesame allergies consumed foods from restaurants that had previously been considered safe but had now added sesame to their dishes.
The situation underscores the importance of clear and accurate food labeling and the need for ongoing awareness about food allergies to ensure the safety of individuals with specific dietary restrictions.
Dr. Ruchi Gupta, a pediatrician and director of the Center for Food Allergy & Asthma Research at Northwestern University, expressed disappointment with the FDA’s decision. While she acknowledges that the decision technically adheres to the law, she had hoped for a more proactive approach from the FDA to support adults and children with sesame allergies by discouraging the widespread addition of sesame to various food products.
The new law, which became effective on January 1, requires all food items produced and sold in the United States to be labeled if they contain sesame. Sesame was designated by Congress as the nation’s ninth major allergen. For years, advocates had been lobbying to include sesame in the list of major allergens, which currently includes milk, eggs, fish, shellfish, tree nuts, peanuts, wheat, and soybeans.
Both the food industry experts and manufacturers expressed the difficulty, cost, and impracticality of completely eliminating cross-contamination risks, leading to the current trend of adding sesame to products and clearly labeling it.
The FDA acknowledged the potential impact of this practice on consumers, but it seems that the agency’s stance on the matter remains unchanged despite the concerns raised by food safety advocates and allergy specialists.
In its response, the FDA acknowledged that the practice of adding sesame to various food products could indeed create challenges for consumers with sesame allergies, and they clarified that companies cannot falsely add sesame to the ingredient list or use statements like “may contain” sesame if it’s not actually present in the product.
Dr. Peter Lurie, the executive director of CSPI (Center for Science in the Public Interest), expressed hope that this clarification from the FDA would serve as a message to food manufacturers. While the FDA is not mandating them to change their practices, it puts the responsibility on the companies to act responsibly and consider the potential risks to consumers with sesame allergies.
As of now, representatives from Wendy’s and Olive Garden have not provided any immediate comments on the matter. It remains to be seen how food manufacturers will respond to the FDA’s stance and whether they will take voluntary steps to address the concerns raised by food safety advocates and allergy experts.